In November, I visited a Manhattan radiology facility for my annual breast examination, and during the administrative process, the receptionist unexpectedly proposed a $40 artificial intelligence scan of my body, which was not covered by insurance.
The offer left me uncertain about its value, and despite feeling somewhat pressured, I declined. However, it did prompt me to ponder the adequacy of my routine mammogram. Why is this AI technology not covered by insurance if it offers such promising benefits?
This scenario is not unique to me. A colleague’s mother recently encountered a similar situation during her mammogram appointment at a remote Baltimore clinic. She was presented with a brochure titled “You Deserve More,” advocating for an AI-enhanced mammogram at an additional cost of $40, which she also declined.
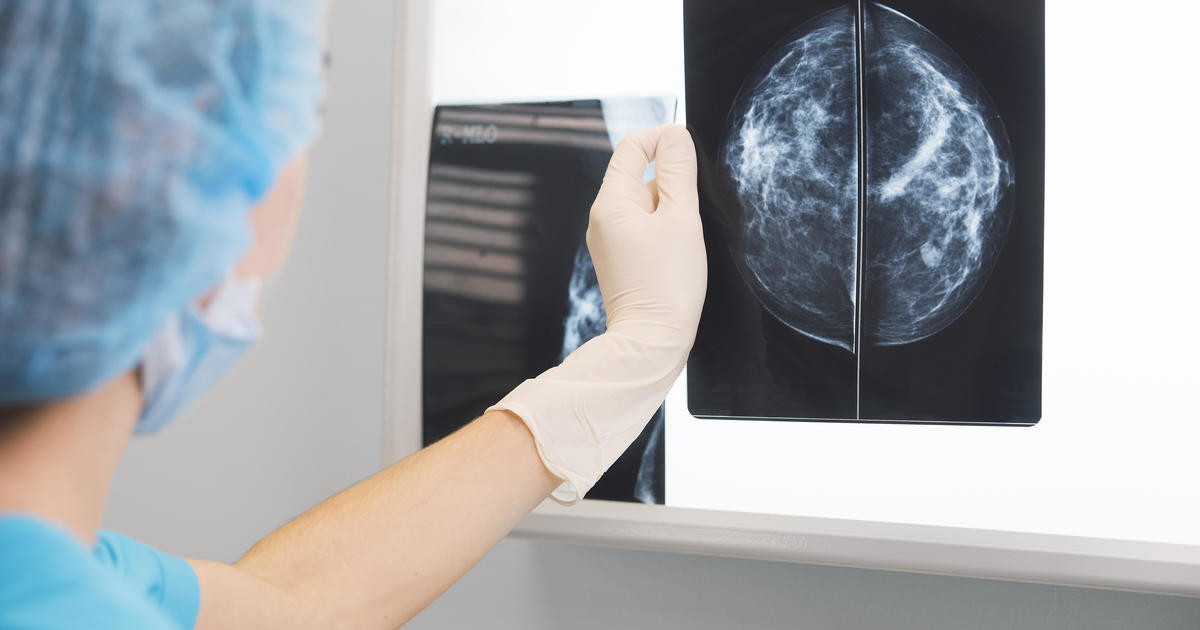
The integration of AI software in radiology for interpreting mammograms has gained traction in medical practice. This technology can analyze extensive image datasets, identify patterns, and detect abnormalities that human radiologists might overlook. By enhancing the identification of suspicious findings, AI has the potential to facilitate earlier detection of breast cancer.
While initial studies show promising results in terms of improved detection rates, some radiologists emphasize the need for further research to ascertain the long-term benefits of incorporating AI into routine clinical practice.
Etta Pisano, a prominent figure at the American College of Radiology, expressed optimism about the potential of AI in radiology but highlighted the necessity for more comprehensive data to evaluate its impact on individual patients.
The radiology centers where my colleague’s mother and I underwent examinations are affiliated with RadNet, a nationwide network of imaging facilities. RadNet introduced its AI mammography product in New York and New Jersey, with plans for further expansion.
Gregory Sorensen, RadNet’s Chief Technology Officer, mentioned a study involving 18 radiologists who evaluated images with and without AI assistance. The results indicated that AI augmentation improved the radiologists’ performance across the board.
The question arises whether the additional cost for AI analysis justifies its clinical utility. The variability in opinions underscores the complexity of this issue.
Laura Heacock, a specialist at NYU Langone Health, suggested that AI could provide reassurance to individuals anxious about their results. However, she emphasized the importance of expert radiologist interpretation as the standard of care.
While mammograms play a crucial role in early cancer detection, they are not infallible, with a reported 20% rate of missed tumors. The FDA has approved approximately 20 AI products to aid in mammogram interpretation, yet the lack of specific billing codes for AI usage poses a challenge for insurance coverage.
RadNet currently charges 35% of patients for AI-enhanced mammograms, while practices like Massachusetts General Hospital do not impose additional fees for AI analysis. Constance Lehman from Mass General highlighted the equity concerns associated with charging patients for AI services.
As the healthcare landscape evolves, the integration of AI in mammography holds promise for improving diagnostic accuracy. However, ongoing research, regulatory considerations, and equitable access remain critical aspects to address in harnessing the full potential of AI technology in breast cancer screening.